HS Damage May Begin Early and Progress Over Time
The majority of patients with hidradenitis suppurativa (HS) have Hurley Stage II at the time of diagnosis, meaning sinus tracts and scarring may have already formed.1,2 One study showed that one-third of those who received an earlier diagnosis at Hurley Stage I already had subclinical sinus tract development.2
As the disease goes undetected or untreated, HS progresses to the formation of extensive sinus tracts, some of which can extend into deeper tissue, including muscle, fascia, and lymph nodes. Assessing sinus tract involvement, scar tissue formation, and psychosocial implications are important aspects of determining disease severity.2,3
52% of HS patients experienced disease progression in 1 or more regions within 2 years in the UNITE registry (N=318).4*
*UNITE: a prospective disease-based registry of patients ≥12 years with active HS. Disease progression defined as a shift in Hurley Stage to a higher stage in any anatomic region compared with baseline (excluding shifts from Hurley 0 to Hurley I).
View Ultrasound Imaging of HS
Gain insight into the deep subdermal damage caused by HS with an ultrasound view of sinus tract development by Hurley Stage. Ultrasound research shows evidence of severe activity under the skin before comparable damage is visible on the surface.2
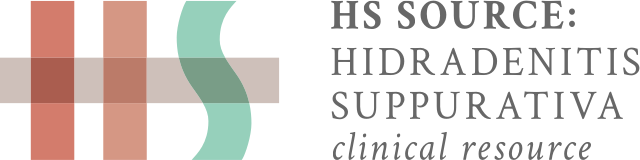
Hurley Stage I
Patient 1: Ultrasound shows dilation of hair follicles2

Clinical image of a case classified as Hurley I
3D ultrasound image demonstrates predominant enlargement of the base of the hair follicles in the deep portion of the dermis.
A Chilean study sought to examine the morphological characteristics of HS using 3D ultrasound to visualize early anatomical changes in HS regions, which may allow the identification of lesions that may benefit from earlier medical treatment and possibly prevent the development of sinus tracts. In this study, ultrasound imaging demonstrated that one-third of patients classified by a certified dermatologist as Hurley Stage I (n=6) were shown to have subclinical sinus tracts.2
Ultrasound shows distortion of the hair follicle preceding perifollicular edema, suggesting that inflammation originates in the follicle.2
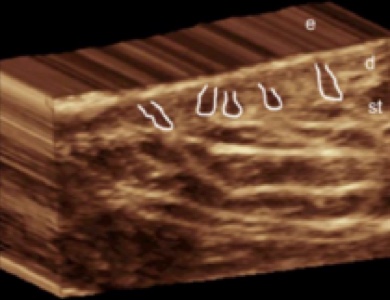
Hurley Stage I
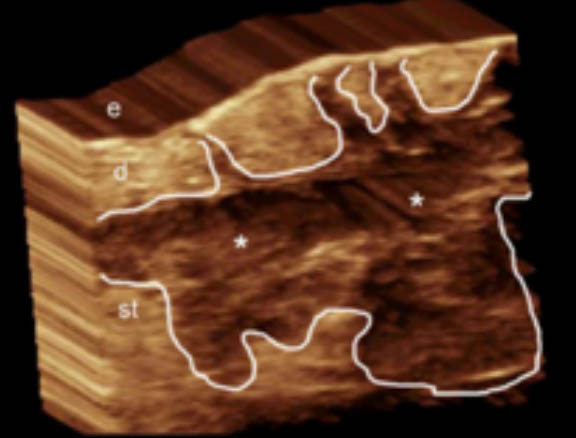
Patient 2: Ultrasound shows a sinus tract2

Clinical image of a case classified as Hurley I
3D ultrasound image demonstrates a sinus tract (* and outlined) that affects the dermis and subcutaneous tissue
A Chilean study sought to examine the morphological characteristics of HS using 3D ultrasound to visualize early anatomical changes in HS regions, which may allow the identification of lesions that may benefit from earlier medical treatment and possibly prevent the development of sinus tracts. In this study, ultrasound imaging demonstrated that one-third of patients classified by a certified dermatologist as Hurley Stage I (n=6) were shown to have subclinical sinus tracts.2
Ultrasound shows distortion of the hair follicle preceding perifollicular edema, suggesting that inflammation originates in the follicle.2
Hurley Stage II
Patient 3: Shows HS at a later stage2
To be kept blank.
3D ultrasound image demonstrates a sinus tract (* and outlined) that affects the dermis and subcutaneous tissue
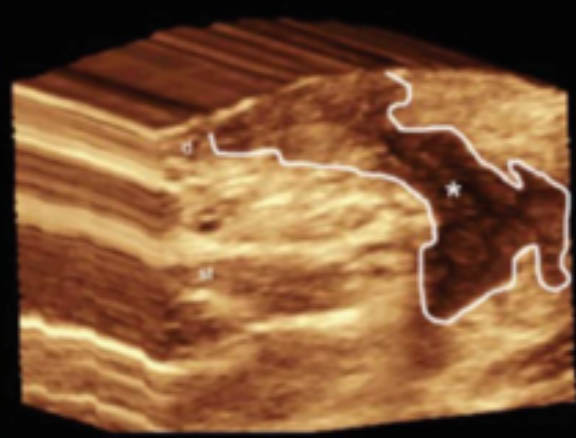
Hurley Stage II
Patient 3: Ultrasound shows the formation of sinus tracts2

Clinical image of a case classified as Hurley II
3D ultrasound image show involvement of multiple hair follicles
These lateral intrafollicular links and the involvement of the base of the hair follicles appear to be the initial steps in the formation of sinus tracts.2
Notice the predominant enlargement of the hair bulbs and the connection between the bulbs (right side of image). The dermis presents increased thickness (white vertical line) and there is a long sinus tract that connects the bottom of a hair follicle with the subcutaneous tissue.2
Blank
Hurley Stage III
Patient 4: Ultrasound shows a large, subcutaneous fluid collection2

Clinical image of a case classified as Hurley III
3D ultrasound image demonstrates a hypoechoic fluid collection (*) with echoes (debris) in the subcutaneous tissue and dermis, also connected to the base of the hair follicles
With more advanced disease, hair follicles are linked to fluid collections and sinus tracts spreading in a linear fashion to the subcutaneous tissue and enlarging to crypt-like structures with progressing disease.2
Notice the complete enlargement and connection of the base of the hair follicles (right half of the image).2
Hurley Stage I
Patient 1: Ultrasound shows dilation of hair follicles2

Clinical image of a case classified as Hurley I
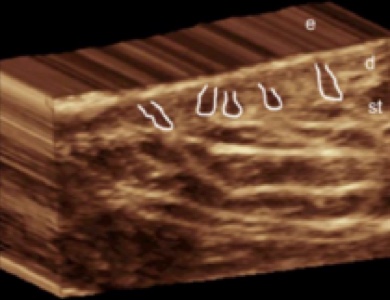
3D ultrasound image demonstrates predominant enlargement of the base of the hair follicles in the deep portion of the dermis.
A Chilean study sought to examine the morphological characteristics of HS using 3D ultrasound to visualize early anatomical changes in HS regions, which may allow the identification of lesions that may benefit from earlier medical treatment and possibly prevent the development of sinus tracts. In this study, ultrasound imaging demonstrated that one-third of patients classified by a certified dermatologist as Hurley Stage I (n=6) were shown to have subclinical sinus tracts.2
Ultrasound shows distortion of the hair follicle preceding perifollicular edema, suggesting that inflammation originates in the follicle.2
Clinical Course of HS
Due to the progressive inflammatory nature of HS, it is proposed that a limited “window of opportunity” exists during which efforts to control HS activity may be most useful. The window may occur during early stages of disease—before the onset of sequelae and before the established disease causes irreversible damage.5
The use of therapeutic options during this window may alter the natural history of the disease by reducing tissue damage.5
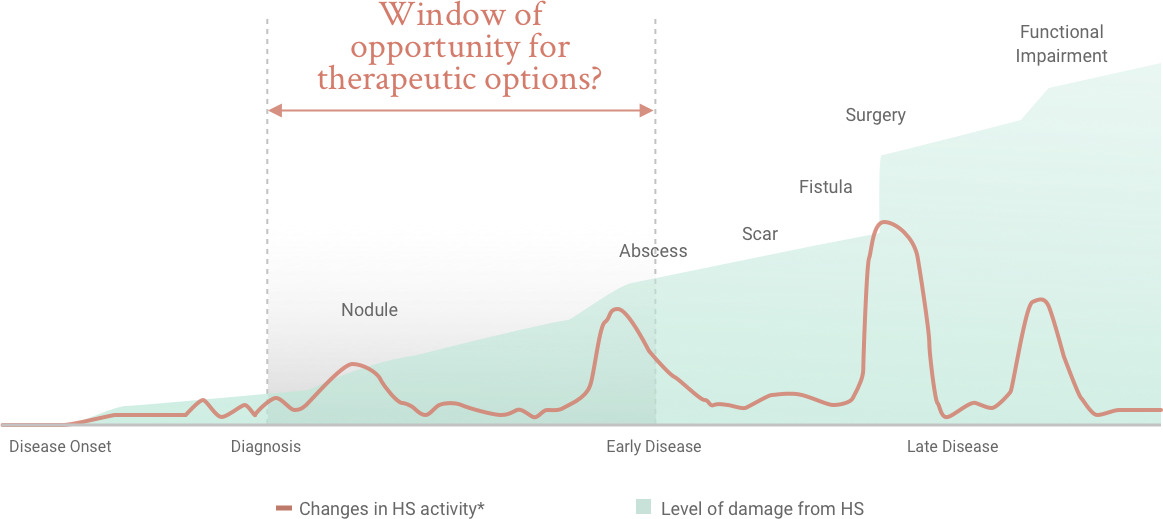
*Changes in HS activity refer to changes in inflammatory activity or symptoms.
HS Treatment Options
There are important considerations when developing a multi-modal management plan.6
Co-managing HS With a Specialist
Partner with an experienced HS specialist in dermatology to co-manage your HS patients.
REFERENCES
1. Jemec GBE. Hidradenitis suppurativa. N Engl J Med. 2012;366(2):158-164. 2. Wortsman X, Jemec GBE. A 3D ultrasound study of sinus tract formation in hidradenitis suppurativa. Dermatol Online J. 2013;19(6). 3. Micheletti RG. Natural history, presentation, and diagnosis of hidradenitis suppurativa. Semin Cutan Med Surg. 2014;33(suppl 3):S51-S53. 4. Kimball AB, Sayed C, Duan Y, Longcore M, Crowley JJ. Characteristics associated with progression of hidradenitis suppurativa (HS): 2-year interim results from the HS UNITE registry. Poster presented at: American Academy of Dermatology Virtual Meeting Experience; June 12-14, 2020. 5. Martorell A, Caballero A, González Lama Y, et al. Management of patients with hidradenitis suppurativa. Actas Dermosifiliogr. 2016;107(suppl 2):32-42. 6. Lockwood SJ, Prens LM, Porter ML, Kimball AB. Treatment of hidradenitis suppurativa. In: Kimball AB, Jemec GBE, eds. Hidradenitis Suppurativa: A Disease Primer. Switzerland: Springer International Publishing AG; 2017:39-51.